Automated Robotic Guidance for Radial Artery Catheterization
Radial artery catheterization is a crucial medical procedure frequently employed in surgeries, intensive care units, and emergencies for catheterization It plays a pivotal role in stent and bypass surgeries. During stent placement, the catheter provides a pathway to deliver the stent to the coronary arteries, effectively treating blockages and improving blood flow. However, the small diameter of the radial artery makes manual punctures challenging. This often leads to failures, complications such as hematomas, and significant patient discomfort.
The success of radial artery catheterization largely depends on the clinician's expertise. Experienced clinicians are more likely to achieve successful catheter placement with fewer attempts, thereby, reducing the risk of complications and improving patient outcomes. However, this introduces variability in outcomes, as less experienced clinicians may struggle with the procedure's technical demands.
Why Automation is Key to Improving Radial Artery Catheterization
The use of radial artery catheterization is expected to increase in the future as it reduces the risk of complications and shortens hospitalization duration. However, the success rate of initial puncture varies significantly depending on the technique. Blind methods (finger pulse detection) have a success rate of 43.9%, while ultrasound-guided methods achieve a higher success rate of 64.8%. for. On average, blind methods require 3.05 attempts compared to 1.65 attempts for ultrasound-guided methods. Similarly, the average puncture time is 108 seconds for blind methods and 88 seconds for ultrasound-guided methods [1].
These statistics underscore the need for improved techniques in radial artery catheterization. Cyient proposes an automated robotic guidance system for radial artery catheterization using ultrasound imaging and advanced kinematics. This innovation has the potential to significantly enhance success rates, reduce the number of attempts, and shorten puncture times, ultimately boosting patient safety, comfort, and procedural outcomes.
System Architecture
Cyient’s proposed automated robotic guidance system for radial artery catheterization integrates hardware and software components to achieve precision, reliability, and safety. The primary goal is to automate with minimal human intervention while ensuring clinical accuracy.

System Components:
- Linear Transducer:
The linear transducer is a critical component, providing real-time imaging and detection of the radial artery. Its ability to capture cross-sectional images of the forearm is indispensable for accurate artery localization.- Flexible Probe Orientation:
- The probe a dynamically adjusts its angle to obtain optimal imaging of the artery from different perspectives.
- This flexibility ensures comprehensive coverage of the scanning area, eliminating blind spots.
- Integration with Robotic Arm:
- The probe is securely mounted on the scanning robotic arm, allowing precise, controlled movements for systematic scanning of the forearm.
- Synchronization with the arm ensures consistent imaging quality while reducing operator dependency.
- Flexible Probe Orientation:
- Syringe Arm:
The syringe arm is engineered for precise needle insertion and alignment, equipped with advanced mobility features to adapt to the radial artery’s orientation with high accuracy.- Vertical Movement: Adjusts dynamically to align with the depth of the artery, ensuring accurate penetration without excessive tissue damage.
- Horizontal Movement: Moves along the forearm to target the puncture site based on the artery’s centroid coordinates provided by the imaging system.
- Yaw Movement: Rotates (yaw) to align the syringe with the artery's orientation, ensuring the needle is positioned at the optimal angle for smooth entry, accommodating anatomical variations.
- Controlled Insertion: Executes steady, controlled movements during needle insertion, minimizing risks such as overshooting or vein collapse.
The combination of these movements makes the syringe arm highly adaptable and reliable for varying patient anatomies and arterial orientations.
- Control Unit:
A centralized controller coordinates the robotic arms using input from the ultrasound probe and image processing algorithms. It ensures synchronization between scanning and puncture operations, reducing delays and improving workflow efficiency. - Inverse Kinematics Engine:
This computational module calculates the joint angles of the robotic arms based on the artery’s centroid location. It enables precise movements while accounting for the needle's orientation, depth and trajectory. - Human-Machine Interface (HMI):
The system includes an intuitive interface for clinicians to monitor and control the procedure. Real-time imaging and feedback ensure the process is progressing as intended. - Redundancy and Safety Mechanisms:
The architecture incorporates fail-safe mechanisms to halt the procedure in case of errors, ensuring patient safety at all times.
Workflow
The workflow outlines a structured method for performing catheterization. Each step aims to enhance precision while reducing human error and patient discomfort.
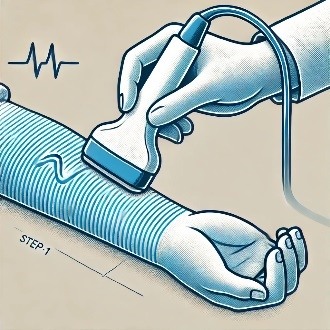
Step 1: Ultrasound Imaging of Radial Artery
The scanning arm moves along the forearm using the ultrasound linear transducer, obtaining images of the underlying anatomical structures. These images are transmitted to a processing unit that filters out noise and enhances the visibility of the radial artery.

Step 2: Image Segmentation and Artery Centroid Detection
Deep learning-based radial artery contour detection is used to segment the artery’s boundary accurately. The centroid of the segmented contour boundary is calculated with sub-millimeter accuracy, ensuring precise targeting for the next steps.

Step 3: Inverse Kinematics and Trajectory Calculation
The inverse kinematics engine uses the centroid coordinates, to determine the optimal joint angles for the syringe arm. The trajectory is then refined to ensure minimal tissue disruption during needle insertion.

Step 4: Needle Insertion
The syringe arm aligns with the computed trajectory and inserts the needle with precision. The system monitors the process in real-time, ensuring accuracy and halting operations if resistance or misalignment occurs.

Step 5: Final Adjustments
After needle insertion, the robotic arm retracts, allowing the clinician to proceed with catheter insertion or other required steps. The system logs all procedural data for future reference and quality assurance.
Benefits
Robotic systems provide various advantages over traditional manual methods, enhancing both procedural efficiency and clinical outcomes.
| Benefits | Details |
|---|---|
| Precision and Accuracy | Real-time ultrasound imaging, combined with robotic control, ensures precise targeting of the radial artery’s center, minimizing first-attempt failures. Sub-millimeter accuracy significantly reduces complications such as hematomas and arterial spasms. |
| Consistency and Reliability | Robotic automation eliminates variability caused by differences in human skill levels, ensuring each procedure follows a consistent, optimized workflow. |
| Reduction in Patient Discomfort | Controlled, steady needle movements reduce pain and anxiety, especially during repetitive procedures. |
| Enhanced Workflow Efficiency | Automation reduces scanning and needle insertion time, letting clinicians focus on other tasks. |
| Data Logging and Analysis | The system records procedural data for quality control, enabling hospitals to monitor outcomes and improve procedural techniques. |
Conclusion
Automated robotic guidance, coupled with real-time ultrasound imaging and inverse kinematics, has revolutionized radial artery catheterization. The precision of these systems ensures sub-millimeter accuracy, significantly reducing first-attempt failures and complications such as hematomas and arterial spasms. By automating the needle insertion process, these systems eliminate variability caused by human skill differences, thus providing a consistent and optimized workflow for each procedure.
Additionally, these advanced systems record procedural data, which is invaluable for quality control. Hospitals can leverage this data to monitor outcomes and refine procedural techniques, ultimately enhancing patient care. As robotic guidance techniques continue to evolve, their applications may extend to other precise medical procedures, further transforming the landscape of medical interventions.
References:
[1] Real-Time Ultrasound Guidance Facilitates Transradial Access, JACC: Cardiovascular Interventions Vol. 8, No. 2, 2015
About the Authors

Amol Gharpure, Senior Solution Architect – Healthcare and Life Sciences
Amol brings over 20 years of expertise in embedded product development, including 15+ years of experience in healthcare domain. His extensive experience spans the entire product development lifecycle of medical devices. Additionally, he has contributed to healthcare robotics by building custom robotic models and has worked in medical imaging, focusing on 2D and 3D image segmentation. His expertise in test fixture design and automation equips him with a strong proficiency in both the development and testing phases of medical technology solutions.

Srinivas Rao Kudavelly, Consultant Senior Principal - Healthcare and Life Sciences
Srinivas has over 25 years of experience which spans across Consumer Electronics, Biomedical Instrumentation and Medical Imaging. He has led research and development teams, focused on end-to-end 3D/4D quantification applications and released several "concept to research to market" solutions. He also led a cross functional team to drive applied research, product development, human factors team, clinical research, external collaboration and innovation. He has garnered diverse sets of skill sets and problem challenges. and has over 25 Patent filings and 12 Patent Grants across varied domains, mentored over 30+ student projects, been a guide for over 10+ master thesis students, peer reviewer for papers and an IEEE Senior Member (2007).
.png?width=774&height=812&name=Master%20final%201%20(1).png)